Nearly two thirds of women aged 45-55 who are experiencing menopausal symptoms say their work has been negatively impacted, according to new research. Should employers be doing more to support female employees through the menopause? Jenny Medlicott speaks to two women about navigating these symptoms in the workplace as well as an expert about what more can be done…
Two years after experiencing her first symptoms of the menopause, fitness instructor Maria Jones went from teaching 25 classes a week to just five.
Life before the menopause was never simple for Maria: she received a systemic lupus diagnosis in 2004 and a kidney transplant in 2014 – and learned that the former increased her risk of early menopause.
But after her kidney transplant, life was better than ever before. Maria found herself running 10ks, going to the gym and cycling frequently, until eventually she turned her love of fitness into a career.
So when she started experiencing all the tell-tale signs of the menopause aged just 41 years old – 10 years before the UK average – it felt abrupt.
“I realised that how I was feeling between classes wasn’t because I was doing too much, it was because of the menopause,” she said.

Maria’s not the only woman whose work life has been knocked off balance by the sudden arrival of the menopause.
In fact, official figures from the British Menopause Society show 42% of women experiencing menopausal symptoms said they were worse or much worse than they expected.
Meanwhile, data from the Local Government Association shows 59% of women aged between 45 and 55 who are experiencing symptoms of the menopause said their symptoms were having a negative impact on their work life.
But why does something which currently affects a third of women in the UK still take so many women by surprise? And are employers doing enough to support these women through this transition in the workplace?
Research suggests not.
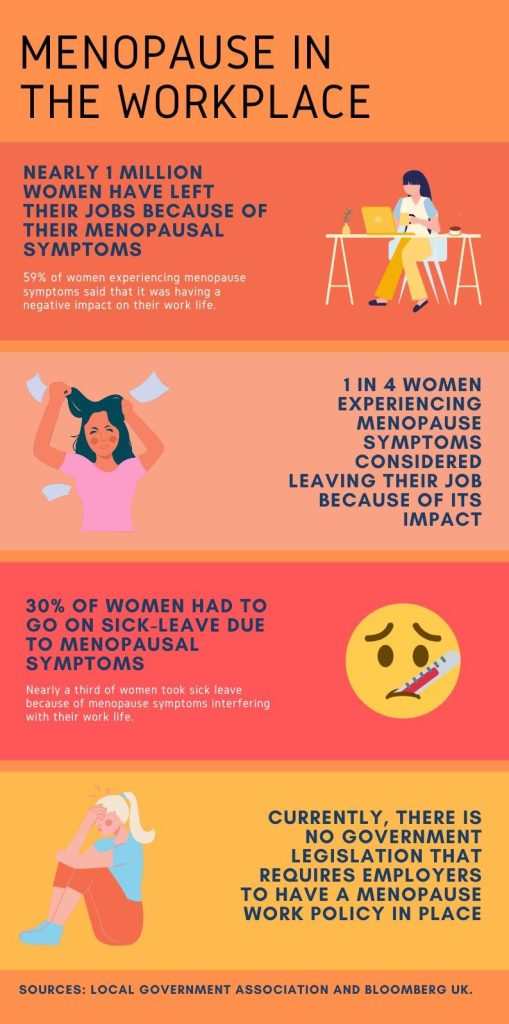
As it stands, currently there is no government legislation in the UK which requires employers to have a menopause work policy in place. That’s despite nearly one million women leaving their job due to the impact of their symptoms of the menopause, according to the LGA.
Dr Louise Newson, menopause specialist and founder of Newson Health, says: “It makes good economic sense to value menopausal staff: employers need to recognise the skills and experience and do everything in their power to retain them.”
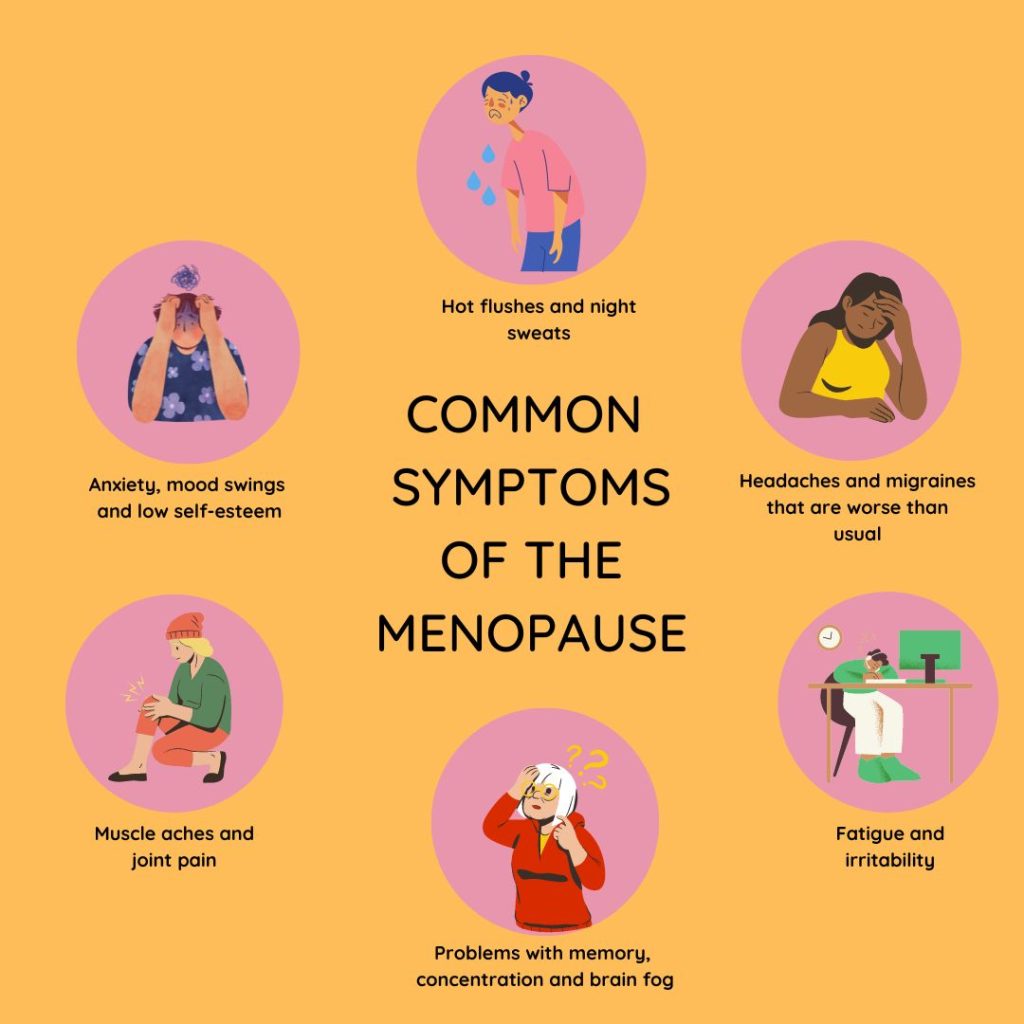
For Maria, at first she tried to resolve her ongoing symptoms herself – constant bleeding, fatigue, headaches, joint pain – by making changes to her work schedule.
But when that failed to make a difference, she sought the help of her GP.
“The GP was very sceptical about the whole thing,” she said. “at that point in time I was only 41 and he said, ‘This is too early, it’s not the menopause.’”
After this, things only got worse.
Maria’s fatigue grew to the point where she was struggling to keep her eyes open while driving, and her reputation in the fitness industry took a hit.
It wasn’t until three years later, in 2021, that the GP finally ran tests to determine it was in fact the menopause which was responsible for her symptoms.
But when gyms started reopening after lockdown, it was already too late. The damage, to her reputation, had been done.
“I tried to get some of my positions back, because I had obviously let them down from giving up the classes – but I didn’t get those classes back,” she said.
Workplace culture in the UK seems to have “a general understanding that women should just get on with it,” she added.
For entrepreneur Claire Winter, perimenopausal symptoms motivated her to change pace in her work life.
Claire’s career prior to the perimenopause was particularly fast-paced.
She was a TV journalist for 20 years, then the editor of a magazine, and later set up a consultancy training business. But once she began suffering symptoms of the perimenopause – the period leading up to the menopause – in 2020, even things which were once second nature, like writing, became a challenge.

“I felt really overwhelmed, found it hard to write, had brain fog, everything became quite tricky,” she said.
“It made me shift away from having a busy consultancy training business because the perimenopausal symptoms were really hard to manage.”
But what would productive action actually look like in the workplace for these women?
“I think it would be useful if people were more open and shared their experiences, like I am,” Claire said.
“So people know they’re not alone, that they’re not going crazy. I still think doctors have got a lot to learn around this.”
As Claire points out, the first step towards helping those who struggle with menopausal symptoms is having conversations. Starting open conversations is one way to chip away at stigma and increase awareness – two foundational tools in the fight for change.
Davina McCall’s 2022 documentary for Channel 4, Sex, Mind and the Menopause and subsequent book, Menopausing: The Positive Roadmap to Your Second Spring, were seen as a significant step forward in this. They kickstarted a cultural conversation which many women have been waiting a long time to have.
Unsurprisingly, her work was met with enthusiasm from those who could relate to McCall’s experience of the menopause.
This, alongside other growing conversations around the menopause, has certainly got the ball rolling.
But it’s only the beginning.
Dr Louise Newson, menopause specialist and founder of Newson Health, said: “There has been a really welcome shift in recent years towards companies becoming more ‘menopause-friendly’, but this has to go beyond providing a few token desk fans to help with hot flushes, and working adjustments like flexible working.
“These measures will not tackle more common symptoms such as low mood, fatigue, memory problems, brain fog and vaginal dryness.
“We need education in the workplace to include information about available treatments, in order for menopausal staff to make an informed decision about their care.
“Staff also need to feel properly supported, so menopause training should be made available to all staff. Just being listened to is so important, and so there should also be dedicated time for colleagues to discuss the menopause, such as support groups.”
Reaching the menopause doesn’t have to be all doom and gloom. Both Maria and Claire have gone onto achieve new and fulfilling roles in their work lives, despite the menopause.
But this doesn’t change the bottom line: menopausal women suffering in the workplace isn’t inevitable – it seems some employers may need to adapt to help future menopausal women cope better with it.
Dr Newson added: “The menopause needs to be treated as everyone’s business, not just those who are menopausal at work.”