A woman sits alone in a busy A&E terrified she will take her own life – because of the severity of her PMS.
To some it may sound like an exaggeration, but it’s not. Premenstrual dysphoric disorder (PMDD), a very severe form of premenstrual syndrome (PMS), is an under-researched chronic health condition facing women across the world.
“Your brain is on repeat like a broken record: ‘you should die, you should die, you should die’,” said Kim Cormack, a playwright who has PMDD.
“I felt like I was going mad.”
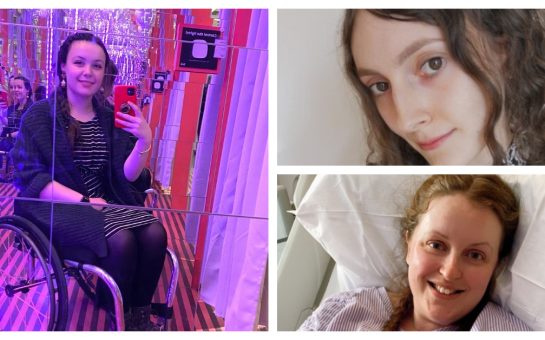
Kim’s story: the battle for diagnosis
Before her PMDD diagnosis Kim felt repeatedly fobbed off. Many male doctors said her symptoms were due to stress. But in 2020, after Kim’s symptoms dramatically worsened, she saw a female GP who referred her to hospital – where she finally felt listened to.
Kim’s difficulty in getting the diagnosis is far from unusual. Dr Rachael Crystal, a general practitioner, explained the difficulties may lie in the amount of symptoms a woman presents with.
She said: “Historically it’s been difficult and challenging for some women to get the support that they need from a healthcare perspective – but I think thankfully that has been changing.
“In the UK there’s a lot of talk around using the term premenstrual syndromes so women aren’t excluded, because the actual diagnostic criteria for PMDD criteria are quite rigid.”
Dr Crystal explained a woman must have five out of 11 set symptoms which affect their life significantly to receive a PMDD diagnosis. This means a person who only records two symptoms may not fit the criteria – even if those symptoms are incredibly severe.
Currently the cause of PMDD is unknown and there is no cure. It is believed to be linked with sensitivity to hormone level changes during a menstrual cycle. Treatments therefore target managing this sensitivity, Dr Crystal explained, such as hormonal treatments like taking the contraceptive pill.
Kim was prescribed Prostap which temporarily stops the ovaries from functioning and therefore the production of oestrogen, which brings on a temporary chemical menopause. Although this helps PMDD sufferers by stopping the normal ovarian hormone cycle, it can cause several severe side effects including hot flushes and decreased bone density.
Kim manages the hot flushes with cool wrap but needs HRT (Hormone Replacement Therapy) due to low bone density.
Despite all this, she considers herself a positive person – even though the suicidal thoughts brought on by her PMDD have meant Kim has had to go to A&E for help several times. Once, the paramedics who arrived to help her had never even heard of the condition.
Kim said: “The main things I think are needed are early education in schools and re-education for medical practitioners about women’s hormonal and mental health.
“Without this it’s impossible to get the mental health support that’s desperately needed to prevent suicide and crisis.”
After trying several treatments Kim is now on a waitlist for a full hysterectomy – an extreme option, but for her potentially life-saving.
Jackie’s story: NAPS
The National Association for Premenstrual Syndromes (NAPS) is 40 years old this year and is run by volunteers like Jackie Howe, CEO.
It provides information to PMS and PMDD sufferers as well as running events for professionals and supporting research into women’s health. NAPS’s last professional conference was a sell-out, and it is working towards setting up hubs across the UK.
Jackie said: “It (NAPS) was set up and at that time there was really only one person providing help for PMS sufferers, a woman called Katharina Dalton.
“We offer advice, support, help and if you take out membership which is very reasonable, £25 for an ordinary member, and it gives you access to a wealth of information.”
She explained that PMDD treatment needs to be tailored to the individual as symptoms are not the same for everyone and this again takes time. At NAPS Jackie has met women who have spent decades trying to be diagnosed – including one who has spent 30 years struggling to get a proper diagnosis.
As well as hormone treatments, doctors may advise making lifestyle changes such as diet and exercise or prescribe antidepressants.
Jackie experienced severe postnatal depression, from which she developed severe PMS. By keeping a diary of her symptoms she could see her worse days coincided with ovulation.
She said: “I had three terrible days, usually depression which struck out of the blue.
“As I might be speaking to you at the moment I would suddenly become severely depressed and then I would have a bad time up to menstruation – and then it would go.”
Jackie stressed the importance of tracking your menstrual cycles and noting down symptoms as there are different patterns. You can track your symptoms in a diary or through a period-tracking app.
It’s this record that can be taken to a GP to prove there is a pattern to your symptoms.
Dr Mahshid Nickkho-Amiry, a consultant gynaecologist and fertility specialist, explained PMDD symptoms include (but are not limited to) suicidal thoughts, lack of energy and anxiety. She added physical symptoms include headaches, achy muscles and joints, and sleep problems.
The symptoms occur during the menstrual cycle’s luteal phase, which is around two weeks in length but can be longer or shorter – this is the time between ovulation and when the period starts.
Phoebe’s story: The PMDD Project
Phoebe Williams set up The PMDD Project, which registered as a charity in April this year, because she didn’t want other women to feel as alone as she did. She had experienced years of struggle, not knowing what was causing her symptoms.
Phoebe has seen a positive shift since receiving her diagnosis but it still massively impacts her life.
She said: “It’s classed as a disability, because it is so debilitating.
“For the week or two – maybe two weeks for me – I can’t function as normal, my thoughts are very different.”
The PMDD Project hosted a Self Love Club event on 4 August at Grub in Manchester. This was the epitome of what the charity stands for – support and awareness – with informative panels and creative group sessions.
Phoebe said: “It was such a joy to see so many people, not just from the PMDD community, come along to our first Self Love Club.
“It was amazing to see people walk in, nervous and unsure about tapping into their creative side, only to leave with newfound confidence and a big smile, happy they tried something new.
“Plus, we were able to signpost anyone struggling with their menstrual cycle to the right help. We can’t wait for the next event!”
When not organising events, The PMDD Project is campaigning to make PMDD a key part of the curriculum in medical degrees, as in Phoebe’s experience she has found numerous GPs don’t know what PMDD is.
Both Dr Amiry and Dr Crystal said there has been an increase in awareness in the area but more needs to be done in terms of research and funding.
Kim became a trustee of The PMDD Project and is now using her PMDD knowledge to develop a community theatre project.
She said: “It will be great actually interviewing other people with PMDD and turning those experiences into a script.”
Resources
When life is difficult, Samaritans are here – day or night, 365 days a year. You can call them for free on 116 123, email them at [email protected], or visit www.samaritans.org to find your nearest branch.
A list of PMDD symptoms and further information can be found on Mind.org.uk and https://www.nhs.uk/conditions/pre-menstrual-syndrome/.
The PMDD Project is focused on raising funding for research into causes, treatments and ultimately a cure. More information on this can be found on their Instagram: @thepmddproject.
Further support and information on premenstrual syndromes can be found on the NAPS website – https://www.pms.org.uk/.
If you are feeling suicidal or are having thoughts of self harm call 999 or go to A&E immediately.
Featured image: © Copyright Katie Aird @ka.social_