This year, the use of Botox injections for the treatment of migraine symptoms marks its 15th anniversary. Although widely known as a cosmetic procedure, the drug isn’t just for pretty faces…
Migraines are one of the oldest ailments known to mankind. The first reported one in history occurred in 1550 BC when it appeared in ancient Egyptian medical documents. Symptoms reported were shooting head pains, visual auras, one sided headaches and relief after vomiting.
The treatment at the time was a ritual involving binding a clay crocodile to the head, intended to provide relief through applying pressure on the scalp.
Luckily, scientific understanding and treatment evolved significantly over the next several hundred years.
In 1926, the drug Ergotamine was introduced as the first medication to treat migraines. However, it had a long list of side effects ranging from nausea to heart problems. This meant it could only be prescribed for patients with infrequent headaches, and was therefore inadequate for chronic long-term sufferers.
Back to the drawing board.
In 1966 scientists reported findings in the use of Propranolol, a beta blocker, after a study of heart pain patients reported experiencing a significant reduction in the frequency of their migraines.
A decade later, beta blockers were FDA (Food and Drug Administration) approved in the US as medication to prevent migraine attacks.
In 1991 the drug Triptan, which prevents pain signals from reaching the brain, became available in Europe. In 2008 it was declared by the American Headache Society as the most important breakthrough in headache medication in 50 years.
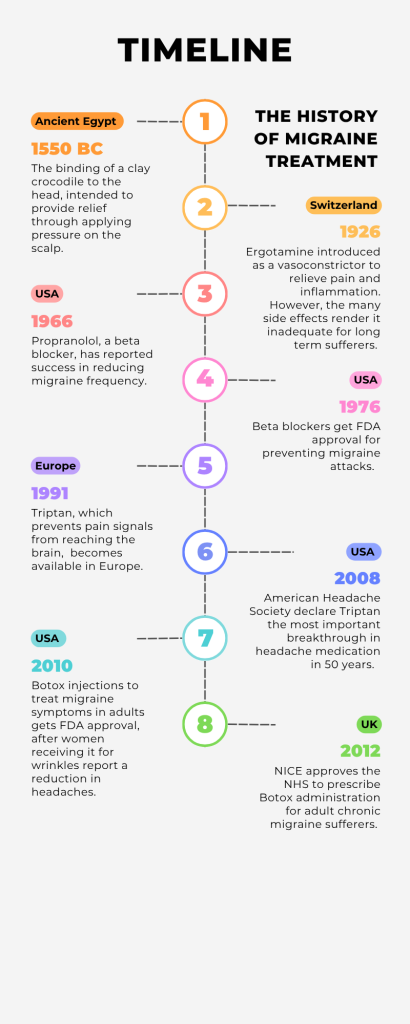
However, our story really begins in the USA, 2010, when the FDA approved Botox injections to treat chronic migraine symptoms in adults.
An accidental discovery, it was made when women receiving Botox for facial wrinkles reported a reduction in headaches. Research trials confirmed it, and NICE (National Institute for Health and Care Excellence) approved it for use in the UK in June 2012.
So, how does it work exactly?
Most people know Botox as a needle injection, typically used to minimize lines and wrinkles. It works to reduce muscle contractions by blocking nerve signals, which relaxes the muscles.
It is much the same principle when used to treat migraines. Botox injections can block pain signals by interfering with the release of neuro transmitters, which are chemicals that transmit pain signals from nerves to the brain.
Anika Kumar, 37, has been receiving Botox injections at Salford Royal Hospital since March 2024 after no other medication provided her with relief.
Prior to this she had been medically signed off work for five years after debilitating migraines prevented her continuing in her career as a dental hygienist.
“I was very nervous as injections always cause a jolt of fear in me, but it’s been a game changer. And as an added bonus, I look younger!”

Image credit: Diana Polekhina on Unsplash
To qualify for the treatment, adults must be diagnosed with chronic migraine, meaning they experience at least 15 days per month with a headache, with at least eight of those days being migraine attacks. Additionally, they must have previously tried at least three other preventive medications that have not worked for them.
The Botox procedure takes place in a 10-15 minute session, and involves the doctor administering around 30-40 injections, typically into the forehead, temples, neck, shoulders and back of the patient’s head. A session happens every 12 weeks, and patients get two sessions to see if the treatment works, and if their migraines decrease.
If so, they continue receiving the injections every three months. If not, their doctor may suggest other preventative medications, such as beta blockers, antidepressants or anticonvulsants.
It has to be said that Botox treatment is not a cure-all, and doctors consider a 30-50% reduction in migraine episodes to be successful. The injections are considered to be a management strategy for migraine symptoms, rather than a preventative measure against attacks.
However, although individual responses vary, according to the National Migraine Centre, approximately 70% of chronic migraine sufferers find Botox injections helpful in reducing the frequency and severity of their migraines by 50%.
“Botox doesn’t dissolve the frequency of my headaches but I’d say it cuts the severity of them in half, and that’s better than anything else I’ve tried,” echoes Anika.
Another recipient of the treatment is Kamila Puton, 28, who began the treatment in April 2025, after having suffered 15-17 migraines a month for upwards of 13 years.
As of June 2025, she has had two rounds of Botox at Salford Royal Hospital, each time receiving 32 injections in her face, scalp, neck and shoulders.
“It takes a few days to start seeing effects, so the first two to three days, I feel completely fine, and then I can tell that I’m losing the ability to move muscles, so around five days after it really kicks in,” said Kamila.
“That’s when my eyebrows really drop down and I struggle to raise them.”
The decreased muscle contractions wear off for Kamila about two weeks before she receives the next round of injections, but so far she has noticed no improvement in the severity of her migraines.
She is set to go in for the third round of Botox in July, and says if that does not produce a result, she will consider her options of alternative treatment, including atogepant, an oral tablet NICE approved on the NHS last year for migraine symptom prevention.
And Kamila isn’t the only one indifferent to Botox administration.
In 2011 the BBC reported that the Drug and Therapeutics Bulletin, which reviews medical treatments in the UK, had conducted a review, and “could not see a place” for administering Botox to migraine sufferers.
The organisation argued that the recent US and UK approved trial of 1,300 patients had included members who were incorrectly diagnosed with chronic migraine, which therefore rendered their successful treatment invalid.
This was challenged by the charity Migraine Action, who publicly stated that they believed sufferers should be offered the option of Botox injections, and that the administration of the drug offered them hope for a better future.
The criticism did not prevent NICE and the NHS from approving the treatment in the UK the following year.
So, while Botox injections for managing migraine symptoms may not be a cure-all, they are considered a significant breakthrough in the field.
Migraines themselves are not fully understood yet, which limits the progress that can be made in treatment therapy, although medical advancements have been regularly achieved since the 1920s, in Europe, the US, and the UK.
And considering the first recorded treatment in Ancient Egypt included clay crocodiles being bound to one’s head, surely any alternative is a better one?
Featured image credit: iStock standard license




