Imagine brain fog so severe that patients report forgetting the day of the week.
Stomach pain so unrelenting that even the strongest medication fails to relieve.
Or fatigue so intense that no amount of sleep can make up for.
Then another 300 known symptoms, all of which have been reported in coeliac disease patients.
The cause?
If a person with this condition consumes even a crumb of gluten-containing food, their body produces an autoimmune response, attacking its own cells, and causing any one of these 300 symptoms to occur.
“My sister was diagnosed after being asked at primary school what her favourite activity was,” recalled Olivia, who also lives with coeliac disease.
“She answered ‘sleeping’.”
And after repeated attacks, the patient is not just put at higher risk for other autoimmune conditions, but also for certain types of cancer.
I was diagnosed with coeliac disease in December 2024 via endoscopy – a procedure that involves sticking a large tube down the patient’s throat and swabbing the inside of their intestine.
Upon receiving my results, I began the sole course of treatment for coeliac disease – a lifelong gluten-free diet.
A month in, I noticed the contents of my wallet being depleted at an alarming rate after each weekly shop.
I began patrolling free-from sections across all major retailers, stunned by the significant rise in pricing for almost every gluten-free alternative.
In July 2024, Coeliac UK found that those on a gluten-free diet pay up to 35% more for their weekly shop than those that are able to eat gluten-containing foods.
Meaning that if a person not on the gluten-free diet pays £150 for food each week, a coeliac disease patient will spend £202.50 on the same basket.
The data was gathered through the recording of over 1000 shopping trips from the Coeliac UK community, sourced from a variety of major supermarkets, and the latest report is due out next month.
But a glance at the shelves in Marks & Spencer shows the cost can be much higher.
I decided to conduct my own research at this supermarket, stocking two separate baskets with eight glutenous items then their gluten-free counterparts.
These items were seeded bread, granola, pasta, soup, cookies, fishcakes, pasta parcels and a ready meal – a deviation from the nutritional standards adhered to in the Coeliac UK report by taking into account luxury items such as sweet treats and fast, easy meals.
The result was a 68% increase in price between the gluten-containing and gluten-free baskets.
Notably, many soups were made with wheat flour in their cheapest, canned forms for as low as 65p, forcing those on the gluten-free diet to purchase £2.75 alternatives.
Sally, a coeliac disease patient from Chichester, said: “My father, who is admittedly a pensioner, moans to me every single week that the price of his bread is now 75p in Aldi.
“It’s incredibly hard to muster up sympathy and I say, ‘Try paying 10-times that for the same amount’ – I find it’s less the cost that irks me than the lack of understanding around it.”
An 800g loaf of brown bread from M&S costs 75p, whereas a 400g free-from brown loaf costs £3.20.
For the same amount of bread, a coeliac disease patient would have to spend £6.40 – almost nine-times the money.
Michael Smith, a coeliac living in a DINK (dual income, no kids) household, gave up on gluten-free alternatives for being “hideously overpriced”, despite being able to afford them if needed.
He said: “If we were closer to the breadline then I would feel forced into changing my diet for financial purposes.”
Smith was more disturbed by the “heavy mental burden” when thinking of where and what he can eat, in the absence of financial worries.
Foods are registered safe to consume for coeliacs if they contain under 20 ppm (parts per million) of gluten, with this amount being adequately tolerated by the majority of those with the condition.
Wheat flour contains gluten ppm in the thousands, meaning an individual with coeliac disease would pass this threshold by consuming a speck the size of a pen tip.
As flour is airborne, many patients have reported being unable to eat in the same room as someone handling flour due to specks being dispersed in near invisible quantities onto their gluten-free meal.
The onus to judge the safety of an environment is placed upon the patient, with factors such as separate cooking spaces, ovens, utensils, plate ware, cutlery and equipment to be considered.
Hannah, 21 from York, said her weekends consisted of “sleeping for hours” pre-diagnosis and this exhaustion was replaced post-recovery by the mental strain of a gluten-free diet.
She said: “Losing that sort of spontaneity was so hard. I couldn’t just go somewhere, walk down a street and find food like my friends could.
“I’d have to pack something in advance, or figure out through my phone where I could actually eat.”
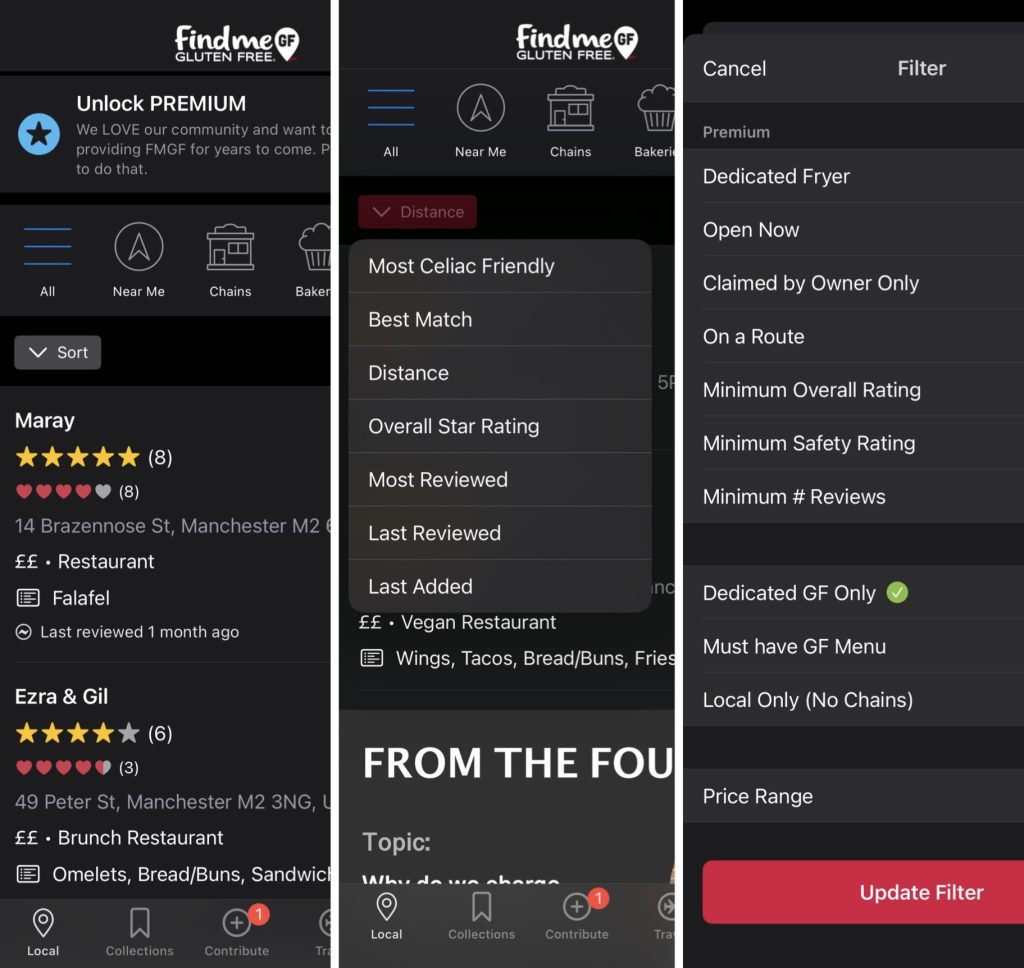
Hannah said that apps such as ‘Find Me Gluten Free’ were crucial in being able to find food on the go – which allows coeliacs to rate restaurants based on safety, taste, price and more.
In the absence of affordable food, and the constant burden of careful consideration when choosing where and what to eat, many coeliacs turn to prescriptions as a means of managing their finances and condition.
Doctors can prescribe those affected with loaves, bread rolls and gluten-free flour – but the patient’s likelihood of living in an area that permits these prescriptions is down to complete chance.
Coeliac UK describes this process as a postcode lottery and estimated that, as of June 2024, roughly 50% of patients living with the condition will reside in an area that provides prescriptions.
This percentage was 80% less than a decade ago, and the decrease in accessibility for patients prompted Coeliac UK to visit 10 Downing Street in March with a petition signed by over 20,000 people supporting prescriptions.
Olivia, a 27-year-old healthcare worker, discussed the changes she’s seen as a coeliac since being diagnosed at the age of three.
Her family of six contains four coeliacs, her mother, two sisters and herself, and Olivia recalled a heavy reliance on prescriptions and the use of a bread maker during her childhood.
She described a significant lack of gluten-free products on the market back then, meaning prescriptions were a necessity for those with the condition.
Olivia said: “It wasn’t as bad financially then because of that support. But things have changed now with prescriptions being taken away, and that hit me hard at university.
“The area I lived in didn’t have them, so bread became a luxury product at £3 a loaf. Having a sandwich was a treat.
To see if your area prescribes gluten-free products through Glutafin, visit here.
The healthcare worker, who is now able on her salary to afford these alternatives, noted that she knows other coeliacs who risk eating products that may contain gluten due to financial instability.
So if patients are opting to poison their own bodies over money worries, when did prescriptions stop being a necessity?
Olivia then described a recent holiday she took with her friend and the precautions she had to take when travelling to accommodate her condition.
She said: “I get stressed when eating out, so I can never leave the house without having something packed. Because if you forget, you might only find something for seven or eight pounds.
“And wherever you’ve gotten food from, you have to think about whether it’s 100% gluten-free or whether you’ve been contaminated.”
Olivia discussed the impact of being a young, female coeliac, which has caused her to receive comments assuming her diet is part of a trend.
She said: “I have a serious autoimmune condition, it isn’t a trend.
“Maybe that’s why companies think they can get away with charging double the price, because they’re adjusting the costs for that portion of the customer base.”
Tristan Humphreys, Head of Advocacy and Public Affairs at Coeliac UK, said: “For too many, the food that keeps those with coeliac disease well is too expensive and hard to access.
“This is bad news for the NHS that has to treat resultant health complications, and devastating for the individuals impacted.”
Coeliac UK believes the solution requires action from not just the food industry, but also from the government, as “prescriptions are a lifeline, not a luxury”.
Andrews said: “We need the food industry to work with us to deliver more affordable and reliable gluten-free staple products in stores, and we’re calling on the UK government to commit to protecting prescriptions.”
Mancunian Matters also spoke with Dr Suneil Raju, a clinical research fellow working with one of the UK’s most well-known coeliac disease specialists, Professor David Sanders.
Dr Suneil said: “It can be really difficult for patients with coeliac disease to access dietary support and there is clearly a need for more.
“The treatment, a gluten-free diet, is challenging and expensive. This means that patients are at a greater risk of a lower quality of life.”
Dr Suneil believes that those with the condition would benefit greatly from access to a dietician with a special interest in coeliac disease, but acknowledged this is challenging to achieve within the NHS.
The clinical research fellow offered a solution when noting that group sessions have been shown to be as effective as 1-2-1 sessions.
Dr Suneil said: “Using webinars could also help to reduce wait times and have less of an environmental impact, as patients can access this from home at a time that best suits them.”
For now, prescription access, the cost and safety of food, and accessing NHS support all remain crucial issues for the coeliac community, yet to be addressed by the government after Coeliac UK’s petition.
After receiving my first prescription for gluten-free products here in Manchester, following months of financial instability, I can’t help but wonder if my support will be the next to go.
To stay updated on Coeliac UK’s mission, visit here.
And to be notified when the next report regarding cost of food is published, sign up to the newsletter today.
Feature image: Kedar Bayley